Introduction
Allogeneic hematopoietic cell transplant (HCT) is a potentially curative therapy for many advanced malignancies; however, it is associated with a significant risk of non-relapse mortality. Several validated measures have been developed to estimate 1-year overall survival (OS) and non-relapse mortality (NRM), but these rely solely on pre-transplant factors to estimate risk. We previously described a “Day 100 risk assessment tool” (PMID 34628474) that aimed to identify the most effective way to deliver high quality care. The score is based on factors primarily occurring within the first 100 days of HCT, demonstrating that, independent of traditional pre-transplant variables, factors identified at day 100 significantly impacted longer term outcomes. This previous analysis included 163 patients who were transplanted from 2015-2018. We now aim to validate our scoring system in a larger, more contemporary cohort.
Methods
The Day 100 risk tool includes 11 binary variables: HCT-comorbidity index ≥ 3, distance from transplant center > 1 hour, day 100 ECOG performance status (PS > 2), acute GVHD requiring systemic corticosteroids, infection requiring intravenous antibiotics, concerns regarding caregiver support, coping skills, substance use, poor health literacy, medication compliance, and “other” concerns from the care team. Patients were given a point for each factor (0 or 1) and total points were summed as the risk score for analysis. Patients who survived at least 100 days were included in analysis. One year survival estimates were analyzed using the Kaplan-Meier method (overall survival [OS]) and cumulative incidence methods (non-relapse mortality [NRM]). Prognostic factors were identified with Cox regression (OS) or Fine and Gray regression (NRM). All patients who died after 1-year were censored at 12 months.
Results
From 1/2018-7/2022, 407 patients underwent first allogeneic HCT and survived at least 100 days without progression of disease. Median age of patients was 61 years old (range 20 - 76) and the majority of patients were: Male (54.3%, N=221), White (88.7%, N=361), diagnosed with acute myelogenous leukemia (AML) (45%, N=183), received peripheral blood stem cells (72%, n=294) had a matched unrelated donor (62.7%, n=255), underwent reduced intensity conditioning (64%, n=259), and received post-transplant cyclophosphamide graft-versus-host disease prophylaxis (52.6%, n=214). Stratified according to best fit for survival, 46.7% (n=190) were classified as “low risk” (0-1), 42.5% (n=173) “intermediate risk” (2-3), and 10.8% (n=44) as “high risk” (≥4) based on Day 100 score.
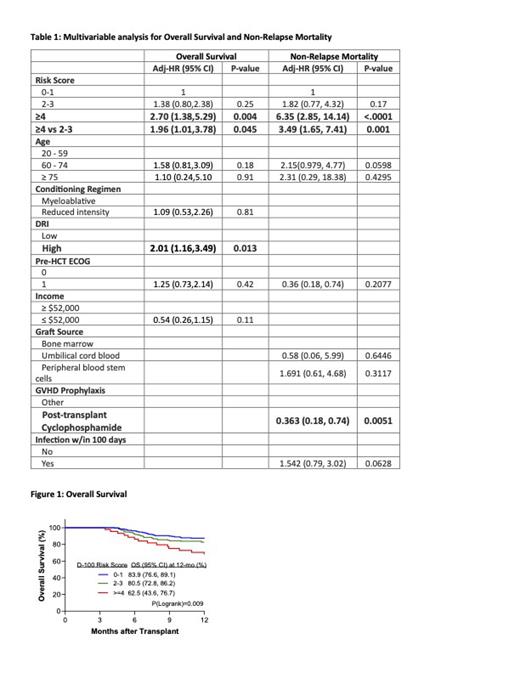
One-year OS was significantly worse for the high risk ≥4) compared to low risk (0-1) and intermediate risk (2-3) (Figure 1). Multivariable analysis demonstrated that the high-risk Day 100 score was significantly associated with 1-year OS and NRM (Table 1).
Conclusion
In a larger contemporary cohort, we validate our Day 100 risk assessment tool as prognostic for 1-year outcomes. Future dynamic scoring systems incorporating post-transplant events may help to identify high risk patients and potential interventions to improve longer-term outcomes.
Disclosures
Sobecks:CareDx: Membership on an entity's Board of Directors or advisory committees. Brunstein:Allovir DSMB: Other: Consultant. Sauter:Juno Therapeutics, Celgene/BMS, Bristol-Myers Squibb, Precision Biosciences, Actinium Pharmaceuticals, Sanofi-Genzyme and NKARTA.: Research Funding; Kite/a Gilead Company, Celgene/BMS, Gamida Cell, Karyopharm Therapeutics, Ono Pharmaceuticals, MorphoSys, CSL Behring, Syncopation Life Sciences, CRISPR Therapeutics and GSK.: Consultancy. Hamilton:Kadmon/Sanofi: Other: advisory board; Equilium: Other: ad hoc advisory board; Therakos: Honoraria; Angiocrine: Other: DSMB; NKARTA: Other: ad hoc advisory board; Incyte: Other: ad hoc consultancy; Rigel: Other: Ad hoc advisory board; CSL Behring: Other: Adjudication committee.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal